Emerging Disruption in U.S. Healthcare: The Long-Term Impact of Extended Telehealth Flexibilities
The recent extension of telehealth flexibilities through 2027 under U.S. federal spending proposals signals more than a temporary policy adjustment. It exposes a weak signal that could ripple through healthcare delivery, workforce management, and insurance models in profound ways over the next decade. As telehealth user numbers rise steadily, and challenges in clinician shortages grow sharper, this regulatory extension could catalyze a far-reaching transformation beyond what is currently anticipated.
What’s Changing?
Federal spending agreements passed by the U.S. House of Representatives have prolonged key Medicare telehealth coverage and associated flexibilities through the end of 2027 (RSM Real Economy). These flexibilities, initially broadened during the COVID-19 pandemic, enable expanded telehealth service reimbursements and regulatory exemptions that would have otherwise expired. Notably, the acute care at home waiver program, which supports hospital-level care delivered in patients’ homes, has also been extended for five years, further cementing virtual care’s foothold (Hillsdale Hospital).
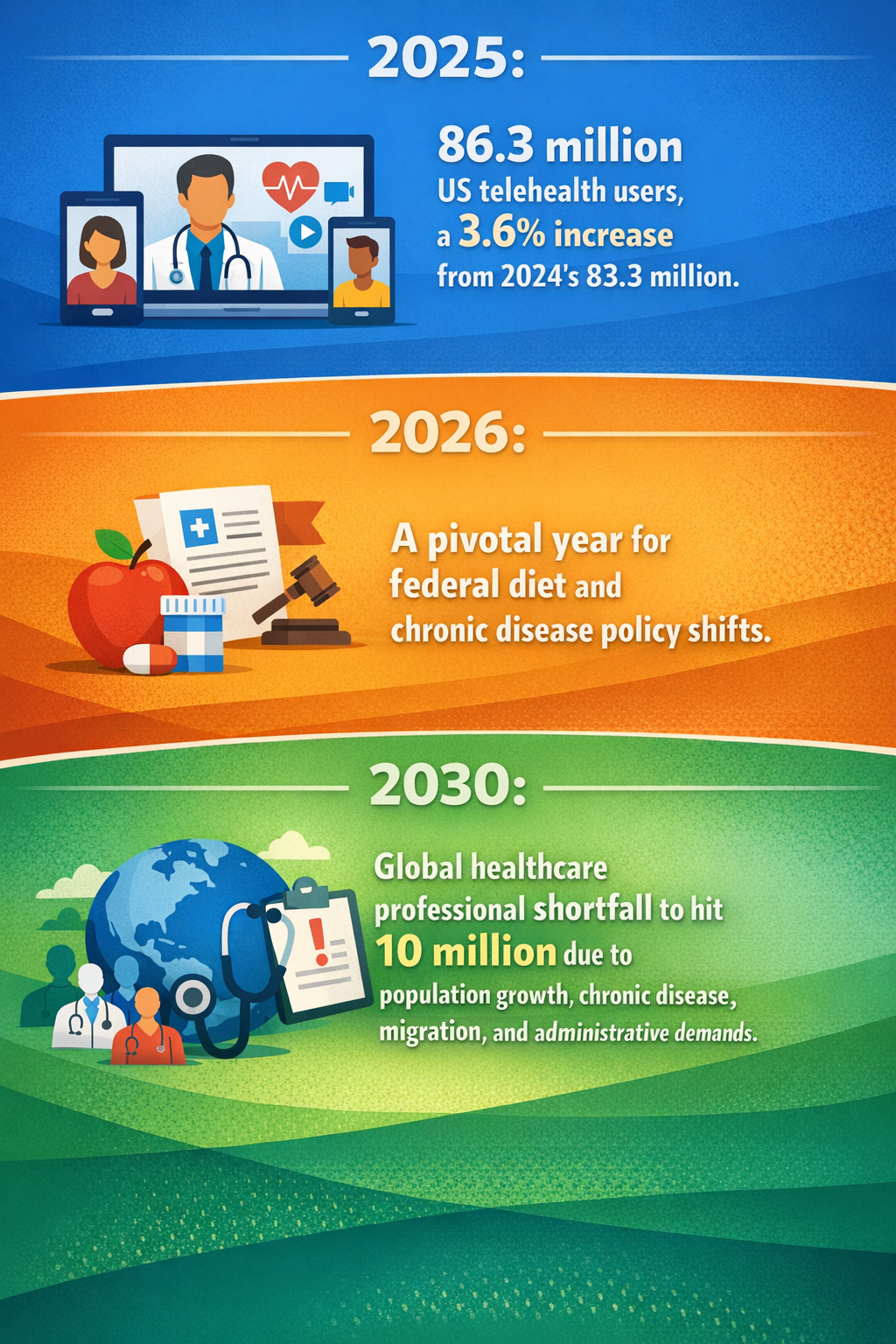
Concurrently, telehealth adoption keeps accelerating. Projections estimate 86.3 million U.S. telehealth users in 2025, an increase of 3.6% over the prior year, driven by new direct-to-consumer telehealth services, pharmaceutical partnerships, and sustained federal support (eMarketer).
Overlaying this expansion are industry-wide headwinds: by 2030, there may be a shortfall of 10 million clinicians caused by population growth, chronic disease prevalence, international migration flows, and increases in clinical administrative burdens (RespoCare Insights). These pressures coincide with a bipartisan policy focus on preventive care, particularly federal momentum on dietary interventions for chronic diseases (UNC News), which could further shift healthcare demand profiles.
In synthesis, these signals—extended telehealth regulatory flexibility, rapid user adoption, clinician shortages, regulatory innovations in home-based acute care, and shifting disease prevention strategies—represent a multi-dimensional change vector that may reshape healthcare delivery and financing well beyond the immediate policy horizon.
Why is this Important?
These developments point to a future where telehealth and remote care move from niche or pandemic contingency models into mainstream, persistently supported pillars of healthcare. The extension of Medicare telehealth provisions reduces regulatory uncertainty, encouraging providers and technology vendors to invest deeper in telehealth infrastructure and innovations.
Workforce shortages in conventional care settings may drive demand for telehealth and home-based modalities, enabling care delivery to expand beyond the physical capacity limitations of hospitals and clinics. Telehealth may evolve into a strategic tool to address clinician scarcity, particularly in rural, underserved, and aging populations.
Furthermore, the growing integration of telehealth into chronic disease management and preventive care could alter insurance models. Payers might increasingly incentivize virtual engagement, focusing on early interventions and continuous remote monitoring rather than episodic in-person treatment. This could disrupt fee-for-service frameworks and catalyze value-based care innovations that rely heavily on digital health data.
For healthcare technology providers and pharmaceutical companies, rising telehealth utilization offers new avenues for patient engagement, data collection, and personalized care pathways. The direct-to-consumer telehealth models gaining traction suggest upstream shifts in how patients choose, access, and pay for healthcare services, affecting traditional provider-patient dynamics.
Implications
Given this constellation of emerging developments, business, government, and healthcare stakeholders should anticipate the following possibilities:
- Accelerated Integration of Telehealth and Home-Based Acute Care: Healthcare systems might rapidly expand offerings of acute-level care at home supported by telehealth, enabling hospital decrowding and cost reductions while enhancing patient comfort and outcomes.
- Redesign of Healthcare Workforce Models: Providers may need to redesign clinician workflows to leverage telehealth effectively, optimizing multidisciplinary collaboration and reducing administrative burdens that currently exacerbate shortages.
- Evolution of Reimbursement and Regulatory Frameworks: Sustained federal support of telehealth could set a precedent encouraging states and commercial payers to codify permanent coverage expansions, shaping a more flexible regulatory environment for remote care technologies.
- Opportunity for Health Data Integration and AI: The growth in telehealth-generated data creates opportunities for advanced analytics and agentic artificial intelligence (AI) systems to support clinical decision-making, risk stratification, and personalized preventive strategies.
- Potential Disruption in Patient Engagement: Direct-to-consumer telehealth offers may erode traditional provider gatekeeping roles, enabling patients to engage with treatment and wellness pathways with greater autonomy and convenience.
- Cross-Sector Collaboration Prerequisite: These shifts might incentivize partnerships between healthcare providers, technology firms, payers, and public health agencies to co-create scalable, secure, and equitable virtual care ecosystems.
However, these opportunities also integrate risks such as exacerbating inequities due to digital divides, concerns about data privacy and security, clinician burnout from virtual care workload, and potential quality gaps if telehealth is inappropriately substituted for in-person care. Strategic planning must weigh these factors carefully to maximize benefits.
Questions
- How can healthcare organizations redesign workflow models to optimize clinician efficiency in a hybrid in-person and telehealth environment?
- What regulatory or payment reforms beyond 2027 would be necessary to sustain telehealth’s integration without compromising patient safety or quality?
- How might telehealth adoption reshape the competitive landscape among healthcare providers, payers, and technology vendors?
- What measures are needed to ensure equitable access to telehealth services across rural, low-income, and aging populations?
- How can emerging AI and data analytics from telehealth interactions enhance prevention and chronic disease management at scale?
- What partnerships or coalition-building across public and private sectors would accelerate secure and effective virtual care ecosystems?
Keywords
Telehealth; Medicare Coverage; Acute Care at Home; Healthcare Workforce Shortage; Chronic Disease Management; Telehealth Regulation; Healthcare Policy Reform; Remote Patient Monitoring; Agentic AI Healthcare
Bibliography
- Under current U.S. House of Representatives spending proposals, key Medicare telehealth coverage and associated flexibilities would be extended through the end of 2027. RSM Real Economy. https://realeconomy.rsmus.com/health-care-industry-trend-watch-week-of-jan-26-2026/
- The 771-page deal does not renew ACA subsidies, but it does extend telehealth flexibilities through 2027 and the acute care at home waiver program for five years. Hillsdale Hospital. https://www.hillsdalehospital.com/news/january-26-2026-what-does-the-great-healthcare-plan-mean-for-rural-hospitals/
- The global shortfall of healthcare professionals will reach 10 million clinicians by 2030, driven by population growth, chronic disease, migration, and the accelerating administrative load placed on medical teams. RespoCare Insights. https://respocareinsights.com/what-agentic-ai-really-means-for-healthcare-in-2026/
- After a year of heightened bipartisan attention to the links between diet and chronic disease, 2026 will be a critical test of whether federal momentum translates into meaningful policy shifts. UNC News. https://uncnews.unc.edu/2026/01/07/unc-experts-share-2026-trend-predictions/
- Key stat: We forecast there will be 86.3 million US telehealth users in 2025, up 3.6% and 83.3 million from 2024. eMarketer. https://www.emarketer.com/content/direct-to-consumer-telehealth-initiatives-grew-2025--fueled-by-pharma--new-services--federal-push